Removing lesions or cancerous tumors often involves extensive surgery, long recovery times, and significant scarring. Thermal ablation is changing how we treat cancer and other lesions. As a minimally invasive procedure, thermal ablation uses extreme temperatures to destroy tumors in targeted areas.
At STARmed America, we’re at the forefront of this innovative technology with our Radiofrequency Ablation (RFA) devices for thyroid and fibroids. Our innovative ELRA Endo Luminal Radiofrequency Ablation catheter helps patients with hepatic, biliary, or pancreatic unresectable endoluminal lesions.
Benefits of Thermal ablation
Part of what makes thermal ablation procedures so innovative is their minimally invasive nature. These procedures are performed through small incisions or natural body openings, utilizing specialized techniques, instruments, and imaging technologies. To ensure patient comfort throughout the procedure, patients will receive mild sedation or local anesthesia prior to the start of the treatment. As a result, patients benefit from less pain, shorter hospital stays, quick recovery times, and reduced scarring comparing to conventional surgeries.
This approach not only enhances patient comfort and outcomes but also lowers the risk of complications and infections, making it a preferred choice for both surgeons and patients for a wide range of medical conditions.
What are the different types of thermal ablation?
Thermal ablation is a medical procedure used to destroy unwanted tissues, like cancerous or benign lesions in different organs like liver, kidney, fibroid and thyroid. The procedure works by applying concentrated heat directly to the target tissue, effectively killing the unwanted cells without the need for traditional surgery.
Thermal ablation encompasses several techniques, each utilizing different energy sources to generate heat for the treatment of diseased tissues. This can include radiofrequency, microwave, laser and high intensity focused ultrasound (HIFU) to target and treat specific areas of concern.
Each of these modalities comes with its unique advantages, limitations and suitability depending on the type, size, and location of the tumor, as well as the overall health of the patient. The choice of ablation method is determined by the treating physician based on these factors. These advanced treatments offer a promising alternative to traditional surgery, aiming to maximize therapeutic efficacy while minimizing harm to healthy tissues.
How Does Radiofrequency Ablation (RFA) Work?
Radiofrequency ablation (RFA) is a type of thermal ablation technique. During a radiofrequency ablation (RFA) procedure, the RF electrode is guided into the targeted area using imaging techniques such as CT or ultrasound scanning for precise placement. To maximize patient comfort from the outset, local anesthesia is administered, paving the way for a pain-free experience.
Once securely in place, the electrode emits radiofrequency (RF) energy, employing high-frequency alternating electrical currents to generate intense heat at the electrode’s tip. This focused heat effectively destroys the unwanted tissues with precision while minimizing risks to the surrounding healthy tissues.
These key aspects of radiofrequency ablation (RFA) help to minimize patient discomfort and significantly shorten recovery times. In most cases, patients leave the hospital the same day as their procedure.
What sets STARmed apart is our commitment to research and innovation, particularly in refining our needles to achieve unparalleled sharpness. This innovative design ensures that our RF electrodes can penetrate the skin smoothly, eliminating the need for an incision, thereby, drastically reducing recovery time, discomfort and the likelihood of scarring.
Radiofrequency Ablation Uses
Radiofrequency ablation is a common treatment for liver tumors. As technology advances, it is also used to treat uterine fibroids, thyroid nodules, and endoluminal cancers.
- Liver tumors: Liver radiofrequency ablation involves inserting a needle into the tumor and destroying tumor cells with radiofrequency waves.
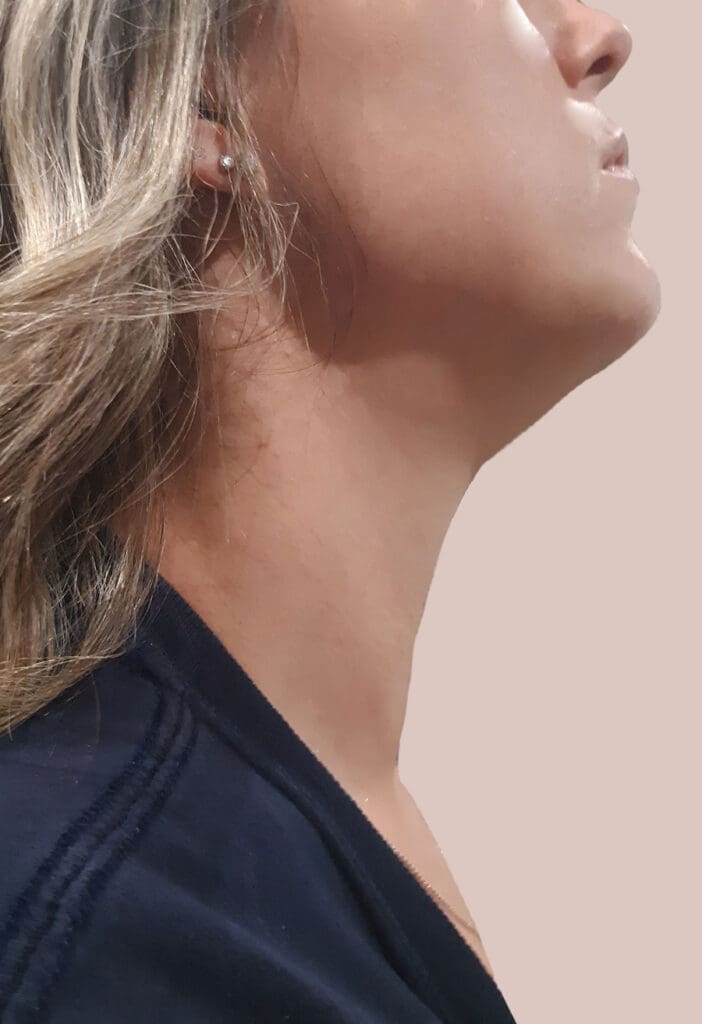
- Thyroid nodules: Thyroid radiofrequency ablation helps destroy lumps in the thyroid gland. A small needle is inserted into the nodule, while radiofrequency waves heat and destroy unwanted nodule tissues.
- Uterine fibroids: Fibroid radiofrequency ablation helps destroy noncancerous uterine growths that cause pain and reproductive disorders. The RF electrode is inserted
- Endoluminal cancers: Endoluminal ablation offers additional palliative care for patients with hepatic, biliary, or pancreatic unresectable endoluminal lesions. Automatic temperature-controlled and flexible RFA electrodes help clear obstructions and tumor growth.
Why Use Radiofrequency Ablation?
Radiofrequency ablation is minimally invasive, effective, and has minimal risk of complications. STARmed thyroid and uterine fibroid radiofrequency ablation technology is non-scarring and incision-free, which helps preserve patients’ healthy thyroid tissue and uterine lining. Avoiding intensive surgery helps improve patient quality of life and recovery time. Endoluminal ablation offers additional palliative care, with minimal damage to delicate bodily structures, when a cure is not achievable.
When it comes to efficacy, the clinical evidence speaks for itself. Research shows radiofrequency is effective and safe when treating thyroid nodules, uterine fibroids, and unresectable endoluminal lesions.
- Observational studies found thyroid nodules treated with radiofrequency ablation had a median volume reduction rate (VRR) of 73% at 6 months and 76% at 12 months.1
- Other observational studies found fibroid radiofrequency ablation had a VRR up to 73.5% after 12 months, with significant symptom reduction just one month after the procedure.2
- Multiple prospective single and multicenter studies show temperature-controlled intraductal RFA helps avoid significant vessel and bile duct injury.3
Is Thermal Ablation the Same as Microwave Ablation?
Microwave ablation is another form of thermal ablation that uses microwave energy. This ablation procedure offers the same benefits as radiofrequency ablation, but it can heat faster to target more extensive areas.4 However, microwave ablation systems may lack the precision in treatment delivery that RFA offers and are not widely available for clinical use. As a result, there are limited studies to prove the effectiveness of microwaves for tumor ablation.5
What to Expect With Thermal Ablation Procedures
Clinical evidence has found thermal ablation is a safe and effective treatment for various conditions. The long-term success of thermal ablation often depends on the type and stage of tumors or lesions. Thermal ablation in early-stage tumors typically has a higher chance of permanently destroying lesions. Advanced tumors may need additional ablation procedures to target the entire area and destroy any progressing lesions.
During Thermal Ablation Procedure

Thermal ablation procedures are often relatively quick, depending on the size and location of the targeted tissue. The procedure is typically performed outpatient, offering a shorter recovery time. Imaging guidance will assist in inserting the thin electrode into the target tissue, and then radiofrequency waves will heat the tissue. This heat breaks down and destroys the tissue.
After Thermal Ablation Procedure
Like all surgeries, patients should be monitored for a few hours after the procedure. Some patients may experience minor pain, swelling, or bruising after thermal ablation. Pain management can help alleviate any post-op discomfort. Usually, you can send patients the same day you perform thermal ablation.
Thermal Ablation Recovery
During recovery, patients should avoid strenuous activities and take pain medication as needed. Follow-up appointments will help manage progress and identify potential complications. Thermal ablation is generally a safe and effective procedure. But, complications can include infection, bleeding, or additional tissue damage.
STARmed America: Your Partner in Ablation Therapy
STARmed America is a leader in RFA technologies. Our thyroid-specific RF electrodes were the first of its kind to enable the introduction of Thyroid RFA in the U.S. The STARmed VIVA combo RF System and star RF electrode have also gained FDA clearance.
Offering minimally invasive treatment options like thermal ablation is crucial in improving your patient care services. At STARmed America, we provide step-by-step guidance on how our technology can integrate into your treatment plans.
STARmed America is at the forefront of revolutionizing patient care, pioneering minimally invasive procedures through the development of state-of-the-art thermal ablation devices. Our commitment to patient experience extends beyond offering cutting-edge technology. Together, we can explore the best path for patient health and quality thermal ablation care.
Contact a STARmed representative to learn more about our RFA technologies.
REFERENCE LIST
- Kandil, E., Omar, M., Aboueisha, M., Attia, A. S., Ali, K. M., Abu Alhuda, R. F., Issa, P. P., Wolfe, S., Omari, S., Buti, Y., Abozaid, O., Toraih, E., Shama, M. A., Lee, G., Tufano, R. P., & Russell, J. O. (2022). Efficacy and Safety of Radiofrequency Ablation of Thyroid Nodules: A Multi-institutional Prospective Cohort Study. Annals of surgery, 276(4), 589–596. https://doi.org/10.1097/SLA.0000000000005594
- Fasciani, A., Turtulici, G., Siri, G., Ferrero, S., & Sirito, R. (2020). A Prospective Intervention Trial on Tailored Radiofrequency Ablation of Uterine Myomas. Medicina (Kaunas, Lithuania), 56(3), 122. https://doi.org/10.3390/medicina56030122
- Laleman, W., van der Merwe, S., Verbeke, L., Vanbeckevoort, D., Aerts, R., Prenen, H., Van Cutsem, E., & Verslype, C. (2017). A new intraductal radiofrequency ablation device for inoperable biliopancreatic tumors complicated by obstructive jaundice: the IGNITE-1 study. Endoscopy, 49(10), 977–982. https://doi.org/10.1055/s-0043-113559
- Gala, K. B., Shetty, N. S., Patel, P., & Kulkarni, S. S. (2020). Microwave ablation: How we do it?. The Indian journal of radiology & imaging, 30(2), 206–213. https://doi.org/10.4103/ijri.IJRI_240_19
- Brace C. L. (2009). Radiofrequency and microwave ablation of the liver, lung, kidney, and bone: what are the differences?. Current problems in diagnostic radiology, 38(3), 135–143. https://doi.org/10.1067/j.cpradiol.2007.10.001





