Summary: Microwave ablation (MWA) is a minimally invasive procedure that uses heat to ablate unwanted tissue, including cancerous tumors. Both radiofrequency ablation (RFA) and MWA provide favorable therapeutic outcomes, with RFA noted for its efficacy and safety, and MWA for its higher ablation power. While microwave ablation (MWA) offers higher power and a larger ablation zone, which can be advantageous for treating larger organs like the liver, this same intensity can pose challenges for smaller, more delicate structures like the thyroid. In thyroid ablation, where precise marginal venous ablation is crucial for effective volume reduction and preventing marginal regrowth, the high power of microwave ablation may increase the risk of complications near critical structures. For this reason, radiofrequency ablation (RFA) is often a safer, more precise option, especially for new practitioners treating thyroid nodules. RFA’s controlled, targeted energy allows for accurate ablation in the thyroid, minimizing risks and preserving nearby tissues.
Microwave ablation (MWA) is a minimally invasive, ultrasound-guided procedure. MWA uses heat to ablate unwanted cells, ranging from benign nodules to cancerous tumors.
The procedure uses a thin, hollow ceramic needle for targeted energy delivery. Most of the time, the physician will start with a small incision using a scalpel on the skin and then insert the antenna. This antenna preserves the surrounding tissue and often eliminates the need for surgical intervention. Along with radiofrequency ablation (RFA), it is one of the most common thermal ablation procedures offered today.
In this guide, we’ll explain the microwave ablation procedure, as well as compare MWA with RFA. Continue reading to learn more about ablation with microwave energy in contemporary practice.
How Does Microwave Ablation Work?
Microwave ablation produces heat via the mechanism of dielectric hysteresis. Subsequently, it destroys targeted tissue using an applied electromagnetic field.
This polar oscillation causes the water in the affected tissue to rotate rapidly, generating heat. Thus, it’s effective on solid organs such as the liver, as well as solid tumors and masses.
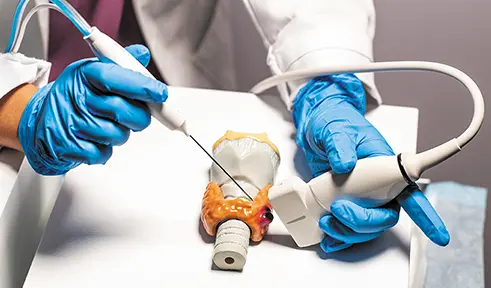
To perform the procedure, physicians need access to a microwave generator and power distribution system. A coaxial transmission line delivers the energy from the generator. Then, clinicians treat the targeted tissue via a ceramic, hollow needle called a microwave antenna. The design of these antennas varies.
The microwave antenna is not sharp enough to penetrate the skin on its own. During ablation, the physician will use a sharp tool such as a scalpel to cut through the skin. By making an incision, the clinician can introduce the antenna into the tissue. Ultimately, this allows them to deliver targeted energy under ultrasound guidance.
The diameter of the needle determines the amount of thermal energy the clinician can deliver to the tissue. Smaller antennas can handle less heat and may increase the risk of burns. However, each antenna is equipped with a cooling mechanism to keep patients as safe and comfortable as possible.
The procedure can be performed in inpatient or outpatient settings under mild sedation or general anesthesia depending on the organ that is being treated. Most patients can return to normal activities within 24 hours of the procedure.
Benefits of the Microwave Ablation The benefits of microwave ablation include:
- Fast heating over a large tissue volume
- Higher ablation power and larger ablation zone
- Low susceptibility to heat-sink effects
- Effective on high-impedance tissue
- Does not require grounding pads
- Minimally invasive compared to surgery
Due to its electrode size, margin of ablation, and temperature range, Microwave ablation is advantageous for certain large organs such as the liver and kidneys.
Disadvantages of the Microwave Ablation
The disadvantages of microwave ablation include:
- Carbonization in ablated tissue due to temperature over 150C
- Lower long-term volume reduction rate (VRR)
- Less friendly to new physicians with less experience in mastering the skill for precise control
- Higher complication rate due to higher power and less control
- Lower precision in ablation due to high power and large ablation zone
- Insufficient marginal venous ablation, which can cause marginal regrowth and lower volume reduction
- Cumbersome coaxial cables
- Higher temperatures increase the chances of unintentional damage to surrounding structures
In many cases, radiofrequency ablation (RFA) may be a safer and more manageable option for smaller, superficial organs like the thyroid, especially for physicians with less experience in thermal ablation.
The tendency toward carbonization alone makes MWA less advantageous on delicate organs such as the thyroid. Carbonized tissue in ablated nodules is difficult to dissolve. This can lead to a lower volume reduction rate (VRR) post-treatment in the long term. The thyroid demands a smaller ablative margin and lower temperature, which is not possible with microwave ablation technology.
RFA uses radiofrequency energy, small, thin electrodes, and lower temperatures. STARmed RFA electrodes are also engineered with exceptional sharpness, allowing for precise puncture without the need for an incision. Additionally, RFA electrodes tend to create more predictable zones of ablation.
STARmed is currently the only company in the market offering the VIVA II Adjustable RF Electrode, a game-changer in thyroid ablation. This versatile electrode features five different active tip sizes, allowing for both precise, controlled ablation around the rim and rapid, large-scale ablation in the center. With this innovation, ablation time for large vascular thyroid nodules is drastically reduced, providing a safe and efficient treatment option. Clinicians can now achieve the precision they need while delivering the faster results patients seek.
In one recent study, the nodular maximal diameter reduction ratio (MDRR) and Volume Reduction Rate (VRR) at six months were significantly better in patients treated with RFA. At later follow-ups, the results remained consistent. Furthermore, RFA functions at temperatures of 110C or less. Thus, the presence of carbonization during a radiofrequency ablation treatment is incredibly rare.
Microwave Ablation vs Radiofrequency Ablation
Some consider microwave ablation to be a form of radiofrequency ablation. However, microwave ablation typically delivers energy at a higher frequency than RFA via direct oscillation of electromagnetic energy. In contrast, RFA uses an oscillating current on the radiofrequency spectrum. Both procedures aim to destroy targeted tissue, which the body naturally eliminates as waste over time.
Microwave ablation is commonly used in the liver. In contrast, radiofrequency ablation is more commonly used on the thyroid, uterus, and pancreas. MWA may be more appropriate for masses or organs with high impedance or low thermal conductivity.
RFA stands out when used in thyroid treatment, however. According to a study done by Dr. Lim and his team, RFA showed a higher VRR at 12 months. It seems to be more suitable for new practitioners and doctors with less experience.
Ultimately, the decision to use MWA or RFA in practice depends on the physician’s training and education. Furthermore, it depends on access to appropriate medical technology.
Microwave Ablation for Thyroid Nodules
Both microwave ablation and radiofrequency ablation are appropriate for the treatment of thyroid nodules. There is little to no difference in patient safety if the clinician has the appropriate training and skillset. However, research suggests that thyroid RFA patients consistently experience more favorable long-term outcomes.
The most current clinical articles suggest that higher VRRs were observed at the 6- and 12-month follow-ups in groups treated with RFA. RFA patients also had a lower regrowth rate than those treated with MWA.
Post-procedure, thyroid patients treated with RFA experience fewer major complications. Compared to those treated with thyroid microwave ablation, RFA patients have both the lowest symptom and cosmetic scores.
As discussed, RFA electrodes tend to be smaller, thinner, and more agile. Lower energy delivery and more predictable ablation margins make it safer to treat delicate nodules. In contrast, MWA remains more advantageous for large organs like the liver.
MWA is also more likely to cause post-procedure voice changes, which can be a negative factor for some patients. In thyroid RFA, 2.8% of patients experienced voice changes. After thyroid MWA, up to 4% of patients experienced this side effect.
However, compared to thyroidectomy, MWA is a less traumatic and invasive procedure with fewer complications. It allows for multiple overlapping ablation zones and is fairly efficient. The shorter length of the procedure makes it more comfortable for patients. As it requires less time and less anesthesia, it is also safer and less costly than surgery.
Step Into the Future of RFA with STARmed America
With the right training, both MWA and RFA are effective in the treatment of benign thyroid nodules. However, when radiofrequency ablation (RFA) and microwave ablation (MWA) are directly compared in thyroid treatments, RFA consistently demonstrates superior Volume Reduction Rates (VRR). RFA also has the advantage of lower complication rates, particularly in preventing voice alterations. This is largely due to RFA’s proficiency in precise margin ablation, allowing for greater control and safety near sensitive structures. Notably, these benefits are even more pronounced for less experienced practitioners, making RFA the preferred choice for clinicians new to thyroid ablation. Contact us to learn more about RFA technology, clinical training, educational resources, and more.





