Thyroid radiofrequency ablation (RFA) is a minimally invasive procedure revolutionizing thyroid care. Unlike traditional surgery methods, thyroid RFA uses precise heat energy to shrink and destroy thyroid nodules caused by thyroid disease. This pinpoint accuracy helps reduce recovery time and preserve healthy tissue.
As medical technology evolves, radiofrequency ablation devices are changing how we treat thyroid lesions. As a result, thyroid RFA has become a safe and effective alternative to traditional surgery. This innovative approach minimizes the risk of damaging healthy tissue and reduces procedural complications.
Let’s explore how thyroid radiofrequency ablation uses precision to treat thyroid nodules without compromising thyroid function.
How Thyroid RFA Works
Thyroid Radiofrequency ablation is intended for percutaneous and intraoperative coagulation and ablation of thyroid nodule tissue. This procedure can help treat thyroid diseases like hyperthyroidism, Graves’ disease, or thyroid cancer in some cases. As a form of thermal ablation, thyroid RFA uses extreme heat to shrink and destroy thyroid nodules that affect thyroid function.
Radiofrequency ablation uses radio waves to generate heat and target thyroid nodules. Guided by an ultrasound, a thin needle electrode is inserted into the targeted nodule. Radiofrequency waves then emit controlled heat into the abnormal tissue. The heat causes the nodule to coagulate and shrink over time.
Unlike surgery, thyroid RFA does not require incisions and general anesthesia. Patients typically can leave the same day they have the procedure. Providers should not use thyroid RFA if patients have pacemakers and other active implants. These implants can lead to energy interference and errors during the RFA procedure.
Clinically-Proven Radiofrequency Thyroid Ablation Benefits
Nearly 20 million Americans live with a thyroid disease that can benefit from radiofrequency thyroid ablation. Clinical evidence shows thyroid ablation is an effective and safe procedure for treating thyroid nodules.
Long-term efficacy: Thyroid Radiofrequency ablation offers long-term nodule reduction and symptom improvement in most patients. Observational studies show thyroid nodules treated with radiofrequency ablation had a median volume reduction rate (VRR) of 73% at 6 months. The VRR increased to 76% at 12 months.1
Minimally invasive: Thyroid RFA doesn’t require incisions or general anesthesia. Nearly two-thirds of thyroid resections treat benign diseases that could have benefited from a less invasive procedure.2 More than 150 clinical articles found that STARmed Thyroid Radiofrequency Ablation (RFA) devices were safe, effective and minimally invasive. No incisions are necessary.3
Precision targeting: Thyroid radiofrequency ablation only targets the nodule, avoiding scarring and damaging healthy thyroid tissue. Preserving healthy tissue helps maintain thyroid function, improving patients’ quality of life and recovery. Thyroid RFA has no to minimal effect on the gland’s functionality.4
Reduced risk of complications: Because thyroid radiofrequency ablation is minimally invasive, it also offers minimal risk of complications. Shrinking nodules with precision heat also reduces the risk of scarring. Some patients may experience minor bruising, swelling, or following ablation. Still, potential side effects are less severe than traditional surgery. Bleeding, infection, and tissue damage after thyroid thermal ablation are rare.5
Speedy recovery: Depending on the size of the thyroid nodule, thyroid radiofrequency ablation procedures are relatively quick. The method is also typically performed in an outpatient setting so patients can be in and out within a day. The minimally invasive nature of thyroid RFA significantly cuts down recovery time.
Radiofrequency Ablation for Thyroid Nodules Outcomes
More than 95 clinical studies support thyroid RFA’s volume reduction efficacy. After follow-up, the volume reduction rate (VRR) of non-functioning benign thyroid nodules (NFBTN) was 80% at 12 months. At 60 months, the VRR was 95%. After a thyroid RFA procedure, patients typically report relief from compressive symptoms. They also retain most, if not all, of the thyroid’s functionality.6
After a radiofrequency ablation procedure, patients should be monitored for a few hours. Some patients may experience minor pain, swelling, or bruising. Creating a pain management plan can help alleviate pain and discomfort. Usually, patients can return home the same day as the procedure. While recovery is often shorter than surgery, patients should avoid strenuous activities and take pain medication as needed.
- Follow-up appointments help review thyroid reduction progress and identify potential complications. Given its clinical efficacy with volume reduction and symptom relief overtime, thyroid RFA is generally a safe and effective procedure.
STARmed America: Your Partner in Precise Thyroid Ablation
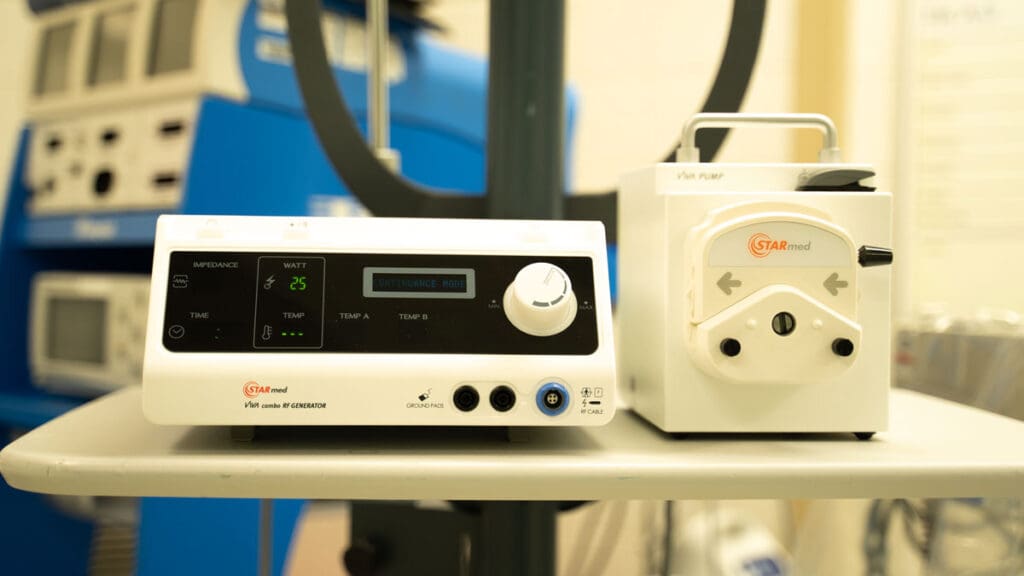
STARmed America is a leader in thyroid RFA technology for safe and effective thyroid nodule treatment. Our monopolar star RF Electrode was the first Thyroid RFA introduced in the U.S. The STARmed VIVA combo RF System is also FDA-cleared for percutaneous and intraoperative coagulation and ablation of tissue:
- The Continuance Mode of the VIVA combo RF Generator constantly produces radio frequency (RF) output while automatically adjusting the amount of energy applied to the targeted nodule based on real-time impedance feedback. This ensures safety by minimizing undesired tissue over-ablation that damages thyroid function.
- The monopolar star RF Electrode offers a range of shorter shaft lengths to accommodate the thyroid gland’s superficial location and a thinner shaft for enhanced, precise energy control. An array of active tip lengths helps providers target different nodule sizes.
- The monopolar VIVA II RF Electrode is the first of its kind. It features an adjustable active tip to accommodate multiple large nodules with one electrode in a single session. Smooth puncture and a smaller handle also allow for greater precision control.
STARmed America is committed to redefining thyroid disease treatment with thyroid RFA technology. We physicians and your care team structured and measured procedure training programs to ensure you can provide the best patient care.
Contact a STARmed representative to learn more about our thyroid RFA technology.
REFERENCES
- Kandil, E., Omar, M., Aboueisha, M., Attia, A. S., Ali, K. M., Abu Alhuda, R. F., Issa, P. P., Wolfe, S., Omari, S., Buti, Y., Abozaid, O., Toraih, E., Shama, M. A., Lee, G., Tufano, R. P., & Russell, J. O. (2022). Efficacy and Safety of Radiofrequency Ablation of Thyroid Nodules: A Multi-institutional Prospective Cohort Study. Annals of surgery, 276(4), 589–596. https://doi.org/10.1097/SLA.0000000000005594
- Kuo, J. H., McManus, C., & Lee, J. A. (2022). Analyzing the adoption of radiofrequency ablation of thyroid nodules using the diffusion of innovations theory: understanding where we are in the United States?. Ultrasonography (Seoul, Korea), 41(1), 25–33. https://doi.org/10.14366/usg.21117
- Vu, D. L., Pham, M. T., Nguyen, V. B., & Le, T. M. (2022). Efficacy and Safety of Radiofrequency Ablation for the Treatment of Autonomously Functioning Thyroid Nodules: A Long-Term Prospective Study. Therapeutics and clinical risk management, 18, 11–19. https://doi.org/10.2147/TCRM.S344464
- Wong, K. P., & Lang, B. H. (2013). Use of radiofrequency ablation in benign thyroid nodules: a literature review and updates. International journal of endocrinology, 2013, 428363. https://doi.org/10.1155/2013/428363
- Lim, J. Y., & Kuo, J. H. (2022). Thyroid Nodule Radiofrequency Ablation: Complications and Clinical Follow Up. Techniques in vascular and interventional radiology, 25(2), 100824. https://doi.org/10.1016/j.tvir.2022.100824
- Jung, S. L., Baek, J. H., Lee, J. H., Shong, Y. K., Sung, J. Y., Kim, K. S., Lee, D., Kim, J. H., Baek, S. M., Sim, J. S., & Na, D. G. (2018). Efficacy and Safety of Radiofrequency Ablation for Benign Thyroid Nodules: A Prospective Multicenter Study. Korean journal of radiology, 19(1), 167–174. https://doi.org/10.3348/kjr.2018.19.1.167






4 Responses
Fantastic blog! “How Thyroid Radiofrequency Ablation Provides the Power of Precision” brilliantly highlights the accuracy and effectiveness of Thyroid RFA. The detailed explanations and patient benefits discussed truly showcase why this minimally invasive procedure is a game-changer for thyroid treatment. Great read!
This article on Thyroid Radiofrequency Ablation is fantastic! I appreciate how it highlights the precision and effectiveness of this treatment. The detailed explanation of how RFA targets thyroid issues with minimal invasiveness gives a clear understanding of its benefits. It’s reassuring to see such advanced techniques improving patient care. Thanks for sharing this insightful piece!
Great post! Your detailed explanation of how thyroid radiofrequency ablation (RFA) ensures precision in treating thyroid nodules is impressive. The ability to target and reduce nodule size effectively with minimal recovery time is a game changer for both patients and clinicians. I also appreciate the emphasis on the benefits of a minimally invasive procedure and how it improves the quality of life for patients. This is a vital step forward in modern medical treatments! Keep up the great work, STARmed!
“STARmed America’s advancements in thyroid RFA technology sound really impressive! The way their VIVA combo RF Generator adjusts energy in real-time to avoid damaging healthy thyroid tissue is a excellent method for patient safety. I also appreciate the design details like shorter, thinner electrodes and adjustable active tips those must make a big difference in precision and comfort during treatment.