TL;DR: Hydrodissection is a key technique in thyroid radiofrequency ablation (RFA), protecting the recurrent laryngeal nerve (RLN) and nearby structures. It creates a fluid barrier to prevent thermal injury, enhancing safety and efficacy.
- Hydrodissection Role: Forms a protective barrier, minimizing nerve damage risk.
- RLN Protection: Reduces chances of voice changes and nerve injury.
- When It’s Needed: Used based on nodule location and anatomical factors.
- Potential Side Effects: Minor swelling, incomplete hydrodissection risk.
- Clinical Efficacy: Studies show significant nodule reduction and fewer complications.
- Training & Support: STARmed America offers hands-on RFA training and clinical support.
Hydrodissection is a key procedural technique utilized in thyroid radiofrequency ablation (RFA). It ensures protection of the recurrent laryngeal nerve (RLN) and the surrounding structures.
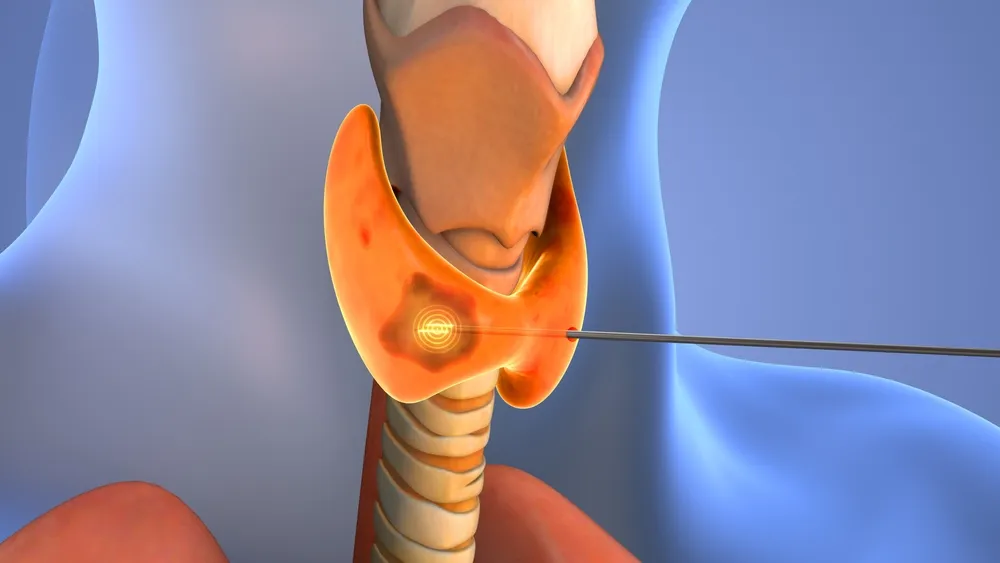
RFA utilizes a small, agile electrode, allowing for incredible precision during the procedure. However, there is still a small risk of thermal injury, making it crucial for clinicians to follow the best procedural practices. The hydrodissection technique is one such practice, enhancing patient safety and outcomes.
In essence, the hydrodissection technique creates a protective barrier between the nodule and surrounding critical structures. This mitigates the likelihood of burns or other damage to the RLN. It’s partially responsible for the low rate of voice changes following the RFA procedure. Thus, hydrodissection is often key to patient satisfaction.
In this guide, we’ll discuss the hydrodissection technique, including its benefits and potential hydrodissection side effects. Plus, we’ll explore its specific role in safeguarding the recurrent laryngeal nerve (RLN) during thyroid RFA. Continue reading to learn how to master this technique and deliver safe and efficacious treatment to your patients.
What is Hydrodissection in Thyroid RFA?
The hydrodissection technique prevents unintended thermal damage from the ablation process. Essentially, it creates a fluid barrier between the thyroid and the delicate surrounding structures, including the RLN. It also protects the patient’s esophagus and nearby blood vessels.
Before the RFA procedure, the clinician will inject a sterile fluid into the perithyroidal space, typically under ultrasound guidance. This fluid serves as a physical barrier and heat sink during the ablation procedure. It effectively pushes the sensitive structures, such as the RLN, away from the zone of ablation.
Since RFA is performed under ultrasound guidance, the clinician monitors the fluid barrier in real-time during the procedure, thus ensuring the fluid layer remains intact.
Hydrodissection and RLN Protection
The thyroid and Recurrent Laryngeal Nerve (RLN) are adjacent structures. Thus, during the RFA procedure, the RLN is particularly vulnerable to injury. The anatomical and physiological factors that contribute to this include:
- The RLN’s proximity to the thyroid gland
- The RLN’s delicate nerve structure
- Variability in RLN anatomy
- Lack of a strong epineurium compared to other nerve structures
- The RLN is prone to secondary nerve damage due to heat conduction through adjacent tissues
If the RLN is injured, patients may experience:
- Neuropraxia leading to transient voice changes
- Axonotmesis requiring weeks to months of recovery
- Neurotmesis potentially resulting in permanent vocal cord paralysis
The hydrodissection technique protects the RLN by:
- Physically moving the RLN away from the ablation zone
- Reducing heat diffusion beyond the ablation zone
- Providing real-time feedback to the clinician during the ablation procedure so they may make adjustments as needed
During Thyroid RFA with hydrodissection, it’s best practice to monitor the patient’s voice function throughout the procedure. This is key for early detection of nerve injury.

When is the Hydrodissection Procedure Necessary?
Clinicians can determine if hydrodissection is necessary on a case-by-case basis. Anatomical considerations, nodule location, and patient-specific factors all play a role.
Typically, the closer the thyroid nodule is to the tracheoesophageal groove, the more likely hydrodissection will be necessary.
Other reasons a clinician may choose to use hydrodissection include:
- The nodule’s proximity to the esophagus, trachea, or major blood vessels
- The size of the nodule and its potential for heat spread to adjacent structures
- The patient presents with difficult-to-distinguish anatomy, and the clinician implements a fluid buffer as a safety measure
In many cases, hydrodissection may not be necessary. Some nodules are small, well-confined within the thyroid parenchyma, and far from the RLN, the danger triangle or other critical structures. However, most experienced thyroid RFA specialists use hydrodissection routinely when treating nodules near the RLN or vital structures.
Hydrodissection Side Effects and Considerations
Ultimately, the benefits of hydrodissection tend to outweigh any risks. Still, patients and clinicians should be aware of the potential complications, including:
- Mild swelling or discomfort that resolves within hours
- The potential for incomplete hydrodissection, which may increase the risk of thermal injury
- Some fluid leakage or absorption, which may slightly reduce the efficacy of the hydrodissection technique
With real-time ultrasound monitoring, however, clinicians can ensure the hydrodissection layer is effective before beginning the RFA procedure. Well-trained clinicians understand they may need to reinject the fluid throughout the procedure to maintain the fluid layer.
With due diligence, it’s possible to reduce or eliminate these risks and keep any side effects minimal.
The Efficacy of Hydrodissection in RFA of the Thyroid
Many clinical studies have found that hydrodissection is both effective and safe for protecting critical structures during RFA.
A recent study found a significant mean nodule volume reduction of 76.3% ± 18.9% at the 12-month follow-up after thyroid RFA with hydrodissection. Symptom and cosmetic scores also showed substantial improvements. A single patient experienced a transient voice change, which resolved within 30 minutes of the procedure.
Furthermore, a study in the Journal of Cancer found that a group receiving hydrodissection experienced fewer complications compared to those who did not, particularly in high-risk nodules, without compromising ablation efficacy.
Finally, a study in the International Journal of Clinical and Experimental Medicine noted a low complication rate following RFA with hydrodissection. The study reported a complication rate of 2.9%. This indicates that the combination of hydrodissection and RFA is a relatively safe and effective approach for managing larger benign thyroid nodules.
Enhance Procedural Efficacy with STARmed America
STARmed America offers comprehensive training programs designed to equip physicians with the skills necessary to perform the hydrodissection technique. Our programs combine theoretical knowledge with practical experience to ensure proficiency in the hydrodissection procedure.
Beyond formal training, STARmed America provides ongoing support through our STAR Support program. We offer clinicians clinical case assistance, reimbursement guidance, and marketing support to help integrate RFA procedures into clinical practice effectively.
For more information on upcoming training sessions and resources, visit the STARmed Academy website.