Summary: Medicare covers radiofrequency ablation (RFA) for benign thyroid nodules if deemed medically necessary. Coverage depends on multiple factors, including diagnostic confirmation and symptom severity. Here’s a quick breakdown:
- Medicare Part B covers 80% of the cost after deductible.
- Medicare Advantage (Part C) covers RFA but may require pre-authorization and network compliance.
- Medical necessity is required—RFA is not covered for cosmetic reasons or small, asymptomatic nodules.
- Repeat treatments are covered if medically justified, though some restrictions may apply.
- Out-of-pocket costs vary based on plan type, deductibles, and copays.
- Check coverage details by calling Medicare or reviewing the plan’s summary of benefits.
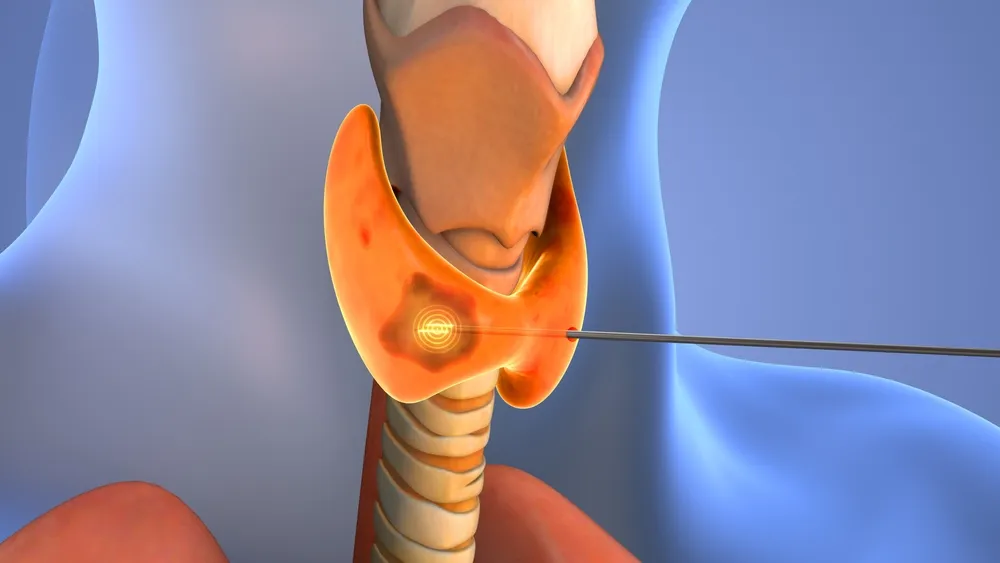
For older patients, thyroid radiofrequency ablation (RFA) may offer a safe way to experience relief from benign thyroid nodules.
Often, these older patients may have other medical complications and are frequently poor candidates for surgery. Thus, Medicare coverage is crucial for older patients who would benefit from a minimally invasive alternative to thyroidectomy.
Many clinicians wonder, “How often will Medicare pay for radiofrequency ablation?” Is it worthwhile to recommend this safe and efficacious treatment option to patients over 65?
In many cases, the answer is yes.
In this blog, we’ll discuss the specific Medicare radiofrequency ablation guidelines that determine coverage. Continue reading to learn how to help your patients qualify so you can optimize their quality of life.
Does Medicare Cover Radiofrequency Ablation?
In short, yes. Medicare does cover the radiofrequency ablation (RFA) procedure when it is deemed medically necessary.
RFA is more commonly associated with chronic pain management. However, its use for thyroid nodule treatment is becoming more recognized in the medical field. This is especially true now that the American Medical Association has granted the procedure a dedicated CPT code.
RFA is categorized under outpatient procedures, which are typically covered by Medicare Part B. However, the procedure must be performed by a Medicare-approved provider and meet specific guidelines.
Medicare Advantage Part C also covers RFA. However, using this coverage may have different requirements for pre-authorization, network providers, and copayments.
However, Medicare’s coverage for thyroid RFA depends on several factors. We’ll outline the specific requirements below.
Medicare Guidelines for Radiofrequency Ablation
Medicare will only cover radiofrequency ablation for the thyroid if the patient and procedure meet specific criteria. This includes:
- Medical necessity. The thyroid nodule must be benign and cause significant symptoms. Medicare does not cover RFA for purely cosmetic reasons.
- Diagnostic requirements. The nodule must be confirmed as benign through fine-needle aspiration (FNA) biopsy or core-needle biopsy.
- Size and symptoms. Medicare may require documentation that the nodule is large enough to cause symptoms. These may include difficulty swallowing, hoarseness, neck discomfort or compression, or visible swelling.
- Failure of conservative treatment. The patient must have tried and failed other treatments before Medicare will approve RFA treatment. Often, these include monitoring and medication.
- Provider and facility eligibility. The procedure must be performed by a Medicare-enrolled specialist in an approved facility.
Regional Medicare policies may also apply. For example, Some MACs may have more restrictive guidelines for covering thyroid RFA. They may require additional diagnostic tests or stricter medical necessity documentation. Furthermore, pre-approval and documentation may vary by region.

How Often Will Medicare Pay for Radiofrequency Ablation?
According to recent research, RFA has a 78% initial success rate. If a nodule does not shrink sufficiently, a second session is typically performed.
Medicare typically covers thyroid RFA on an as-needed basis. That means repeat treatments are typically approved if deemed medically necessary. With that said, some MACs impose limits on how frequently the procedure can be repeated within a specific time frame.
Clinicians should ensure that a patient’s medical records support additional treatments when necessary. If a nodule regrows or additional nodules develop, the physician must document the need for another RFA session.
Radiofrequency Ablation Cost with Medicare
RFA is covered by Medicare, but multiple factors contribute to how much radiofrequency ablation costs.
With Medicare Part B Coverage
Medicare Part B covers 80% of the Medicare-approved amount after the patient meets their annual deductible. The patient is responsible for the remaining 20% of costs. The exception is if they have Medigap insurance, otherwise known as Medicare Supplement insurance. Medigap may cover some or all of the remaining 20% of treatment costs.
With Medicare Advantage Part C Coverage
Medicare Part C is required to cover what Medicare Part B covers. However, the cost of thyroid RFA with Medicare Advantage can vary based on several factors. These include the plan’s copayments, deductibles, and provider network rules.
The out-of-pocket cost for thyroid RFA with Medicare Part C depends on:
- Whether or not the plan has a monthly premium
- Whether or not the patient has met their annual deductible
- Whether the plan charges a fixed copay or uses a coinsurance structure
- Whether it is an HMO or PPO plan
How to Find the Exact Out-of-Pocket Cost for Thyroid RFA
With Medicare Part C, have your patient check their plan’s summary of benefits. There, they’ll find their specific coinsurance and copay amounts.
The fastest way to get an answer is to have them call their Medicare provider. The phone number is typically located on the back of the insurance card. Once connected, they can directly ask about RFA coverage.
With Medicare Part B, the process is simpler. There is now a dedicated CPT code for Radiofrequency Ablation of the thyroid. Using the code, patients and clinicians can request the exact Medicare reimbursement rate.
Treat More Patients with STAR Support
STARmed America is the only company that offers exceptional service packages to our participating clinicians. That includes ongoing reimbursement support. This ensures your patients can afford the most effective, least invasive treatment for their benign thyroid nodules.
Learn more about Thyroid RFA and how we can support you in improving the quality of life of all patients.